How Often Do You Need to Take a Tb Test

Baseline TB Screening and Testing
All U.S. health care personnel should be screened for TB upon hire (i.e., preplacement). TB screening is a process that includes:
- A baseline individual TB risk assessmentpdf icon ,
- TB symptom evaluation,
- A TB test (e.g., TB blood test or a TB skin test), and
- Additional evaluation for TB disease as needed.
Information from the baseline individual TB risk assessmentpdf icon should be used to interpret the results of a TB blood test or TB skin test given upon hire (i.e., preplacement). Health care personnel with a positive TB test result should receive a symptom evaluation and a chest x-ray to rule out TB disease. Additional workup may be needed based on those results.
Health care personnel with a documented history of a prior positive TB test should receive a baseline individual TB risk assessment and TB symptom screen upon hire (i.e., preplacement). A repeat TB test (e.g., TB blood test or a TB skin test) is not required.
Annual Screening, Testing, and Education
Annual TB testing of health care personnel is not recommended unless there is a known exposure or ongoing transmission at a healthcare facility. Health care personnel with untreated latent TB infection should receive an annual TB symptom screen. Symptoms for TB disease include any of the following: a cough lasting longer than three weeks, unexplained weight loss, night sweats or a fever, and loss of appetite.
Healthcare facilities might consider using annual TB screening for certain groups at increased occupational risk for TB exposure (e.g., pulmonologists or respiratory therapists) or in certain settings if transmission has occurred in the past (e.g., emergency departments). Facilities should work with their state and local health departments to help make these decisions.
All health care personnel should receive TB education annually. TB education should include information on TB risk factors, the signs and symptoms of TB disease, and TB infection control policies and procedures. TB education materials can be found through CDC, the TB Centers of Excellence for Training, Education, and Medical Consultation, NTCAexternal icon, State TB Programs, and the Find TB Resources website.
Post-Exposure Screening and Testing
All health care personnel with a known exposure to TB disease should receive a TB symptom screen and timely testing, if indicated.
- Health care personnel with a previous negative TB test result should be tested immediately and re-tested 8 to 10 weeks after the last known exposure. For consistency, the same type of TB test (e.g., TB blood test or TB skin test) should be used upon hire (i.e., preplacement) and for any follow-up testing.
- Health care personnel with a documented history of a positive TB test result do not need to be re-tested after exposure to TB. They should receive a TB symptom screen and if they have symptoms of TB, they should be evaluated for TB disease.

Baseline Testing
The process for baseline testing using a TB blood test is as follows:
- Administer TB blood test following proper protocol
- Review result
- Negative — consider not infected
- Positive — consider TB infected and evaluate for TB disease*
- Document result
Using a TB blood test for baseline testing does not require two-step testing. Additionally, TB blood tests are not affected by the BCG vaccine.

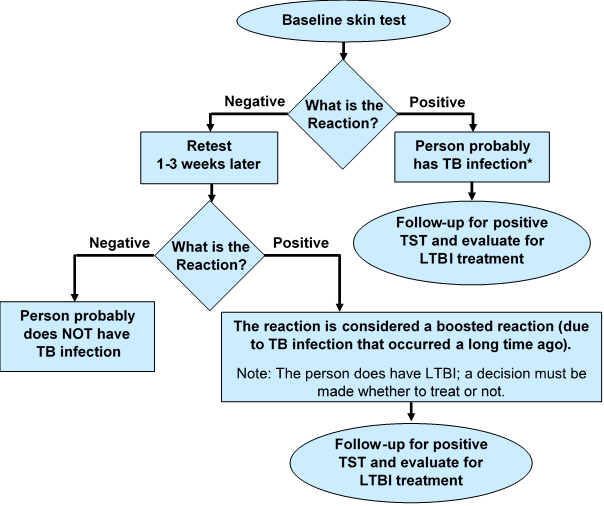
Baseline Testing: Two-Step Test
If the Mantoux tuberculin skin test (TST) is used to test health care personnel upon hire (preplacement), two-step testing should be used. This is because some people with latent TB infection have a negative reaction when tested years after being infected. The first TST may stimulate or boost a reaction. Positive reactions to subsequent TSTs could be misinterpreted as a recent infection.
Step 1
- Administer first TST following proper protocol
- Review result
- Positive — consider TB infected, no second TST needed; evaluate for TB disease.*
- Negative — a second TST is needed. Retest in 1 to 3 weeks after first TST result is read.
- Document result
Step 2
- Administer second TST 1 to 3 weeks after first test
- Review results
- Positive — consider TB infected and evaluate for TB disease.
- Negative — consider person not infected.
- Document result
Two-Step TST Testing
How Often Do You Need to Take a Tb Test
Source: https://www.cdc.gov/tb/topic/testing/healthcareworkers.htm